Lupus: The Disease of 1,000 Faces
May is Lupus Awareness Month, so we’re sharing facts about this disease that commonly goes undiagnosed.
According to the Lupus Foundation of America, up to 1.5 million people in the U.S. may be living with lupus, with nearly 16,000 new cases reported each year. Lupus can be difficult to diagnose because its symptoms often mimic other ailments. Due to its complicated nature, lupus is sometimes called the “disease of 1,000 faces.”
What is lupus?
Lupus is an autoimmune disease in which the body’s immune system attacks its own healthy tissue and organs. This long-term condition can affect many different body systems, including skin, joints, blood cells, kidneys, brain, heart and lungs. The chronic nature of lupus means it typically lasts longer than six weeks and often for many years. Although lupus can range from being mild to life-threatening, with proper medical care, most lupus patients can live a full life.
What causes lupus?
Lupus is an autoimmune disease, yet the exact cause is unknown. A combination of genetics and environment likely causes lupus.
A healthy immune system will protect the body by fighting off antigens, such as bacteria, viruses and germs. It does this by generating proteins called antibodies, produced by white blood cells. In a person with an autoimmune condition, such as lupus, the body cannot distinguish between harmful substances, or antigens, and healthy tissue. As a result, the immune system sends antibodies to fight against both the antigens and healthy tissue. This results in inflammation, pain and tissue damage.
What are the symptoms?
The signs and symptoms of lupus vary significantly among patients, and no two cases are alike. The most common symptoms include:
- Fatigue
- Fever
- Chest pain
- Dry eyes
- Shortness of breath
- Headaches, confusion and memory loss
- Joint pain, stiffness and swelling
- Skin lesions that appear or worsen with sun exposure
- Butterfly-shaped rash on the face that covers the cheeks and bridge of the nose or rashes elsewhere on the body
- Fingers and toes that turn white or blue when exposed to cold or during stressful periods
Symptoms can develop slowly or may come on suddenly. Cases can range from mild to severe and may be temporary or permanent.
Most people with lupus experience mild disease symptoms during episodes, called flares. These flares occur when symptoms get worse, then improve or disappear entirely for a period of time. Lupus symptoms also depend on which body system is affected by the disease.
Who is at risk for lupus?
According to the Lupus Foundation of America, lupus occurs more frequently in women. In fact, women are nine times more likely to develop lupus than men. Historically, lupus is more common in African-Americans, Hispanics and Asian-Americans. Lupus can affect people of all ages, though it is most often diagnosed in individuals ranging from 15 to 45 years old.
How is lupus diagnosed?
Lupus can be difficult to diagnose because the signs and symptoms so closely resemble those of other illnesses. Underdiagnosis of lupus often occurs. Unfortunately, there is no one test to diagnose lupus. Doctors will use a combination of blood and urine tests, symptom discussions, physical examinations and family history to diagnose the disease.
What is the treatment for lupus?
Treatment for lupus is an ongoing process and depends on the symptoms. Discussions with your doctor will determine how your symptoms will be treated. Medications most commonly used to control lupus include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Antimalarial drugs
- Corticosteroids
- Immunosuppressants
- Biologics
- Rituximab
How can I cope with lupus?
Coping with the on-going effects of lupus can be a difficult task and extremely frustrating at times. Learning all you can about the disease and having discussions with your doctor can help you take control of your treatment. Effective therapy to help manage symptoms can help lupus patients maintain a healthy and active lifestyle. Raising lupus awareness, along with upport and understanding from family and friends, are essential components of coping with the disease.
Where can I get treatment for lupus in the Triangle?
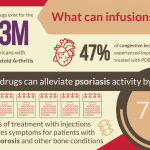
Personalized Hematology/Oncology’s certified infusion center offers intravenous treatment for rheumatology-related autoimmune conditions, including lupus and arthritis. We work closely with your primary physician to determine the course of treatment that will work best for you and your lifestyle.
June is Lupus Awareness Month. If you or a loved one are experiencing symptoms that resemble those of lupus, consult with your primary care physician for an assessment, or schedule an appointment with our in-house primary care doctor who is also a lupus treatment specialist.